

Introduction
Presently, I am employed on a full-time basis in the Intercounty Gaelic Games (Offaly GAA) in Ireland. My primary responsibility is to
deliver specialised strength and conditioning programs to the Senior Football and Hurling teams, with a focus on
rehabilitation. In the past, I worked as a physiotherapist in both clinical and hospital settings. Working as a Rehab
Coach within an elite athletic context provides fresh challenges in compared to working within more frequently established sectors of
therapeutic practice such as the HSE/NHS or private practice. The traditional doctor-patient relationship, commonly observed in
conventional settings, faces a new challenge in the realm of sports with the introduction of the doctor-patient-team
relationship.
The primary ethical dilemmas that might impact decision-making in sports include confidentiality, informed consent, equitable competition,
anti-doping measures, involvement of third parties, and the use of cutting-edge technology. The Sports Physiotherapy Competency Standards
highlight the need of cultivating professional conduct that guarantees the responsibility to provide care in situations when conflicts of
interest may arise. The primary goals of Physiotherapy / Rehabilitation for non-athletic individuals often revolve around promoting
long-term functional recovery and minimising outcome measures such as pain. Within the sporting environment the primary focus for
athletes is typically the speed of their recovery, with the possible long-term health risks being of secondary relevance compared to their
sports achievements.

This principle is reflected in our medical and rehabilitative strategy, as one of our primary metrics for assessing the effectiveness of our team is the duration it takes for athletes to return to play after injury or surgery. The primary cause of ethical lapses is typically a clash between the well-being of the player and the desire for optimal performance, rather than a lack of comprehension on the part of the doctor. Previous pitfalls in this area have been highlighted with the return to play times of athletes suffering from concussions. Medical practitioners must utilise their clinical expertise to make decisions in the best interest of their patients. Some have said that the primary moral obligation of a sports physician is to prioritise the well-being of the athlete patient. However, numerous sports physicians also have a sense of duty to prioritise the interests of the team (such as a club or franchise) they are employed by.
There may be instances where a Rehab Coach deviates from their core responsibility of ensuring the player's health and becomes engrossed in the mindset of a fan. They could acquire a feeling of duty towards the team's accomplishments, which could have a detrimental impact on the impartiality of their decision-making. In order to deliver superior treatment in a high-level sports setting, it is crucial to maintain constant awareness of rules and legal modifications set out by our regulating organisations. The process of making ethical decisions in the medical field can be susceptible to several influences, including external demands from coaches, athletes, and the physicians themselves.
An illustrative instance of this during Gaelic Games is when a player, who sustains a hamstring strain during a match, faces coercion from
the coaching staff to resume playing despite being in pain or having loss of function. Historically, players who demonstrated an inability
to make a definitive choice would persist in participating in the game despite receiving recommendations against it from medical
professionals. The Gaelic Athletic Association has issued recent medical recommendations that mandate players to adhere to a prescribed
phased return to play route after being diagnosed with a concussion. Within our environment there has been educational sessions to the
coaches and players elucidating the updated protocols for managing concussions, with the aim of reducing the likelihood of any
disagreements. Additional guidelines and channels from our regulating authorities are necessary to effectively mitigate ethical
concerns. This article will examine the primary tasks and obligations that are unique to a Rehab Coach in the context of Gaelic Games.
It will also analyse how these roles and responsibilities are affected and reinforced by evidence-based practice and clinical
governance.
The Medical, Performance & Coaching Team
Figure 1: Communication channels within Offaly GAA
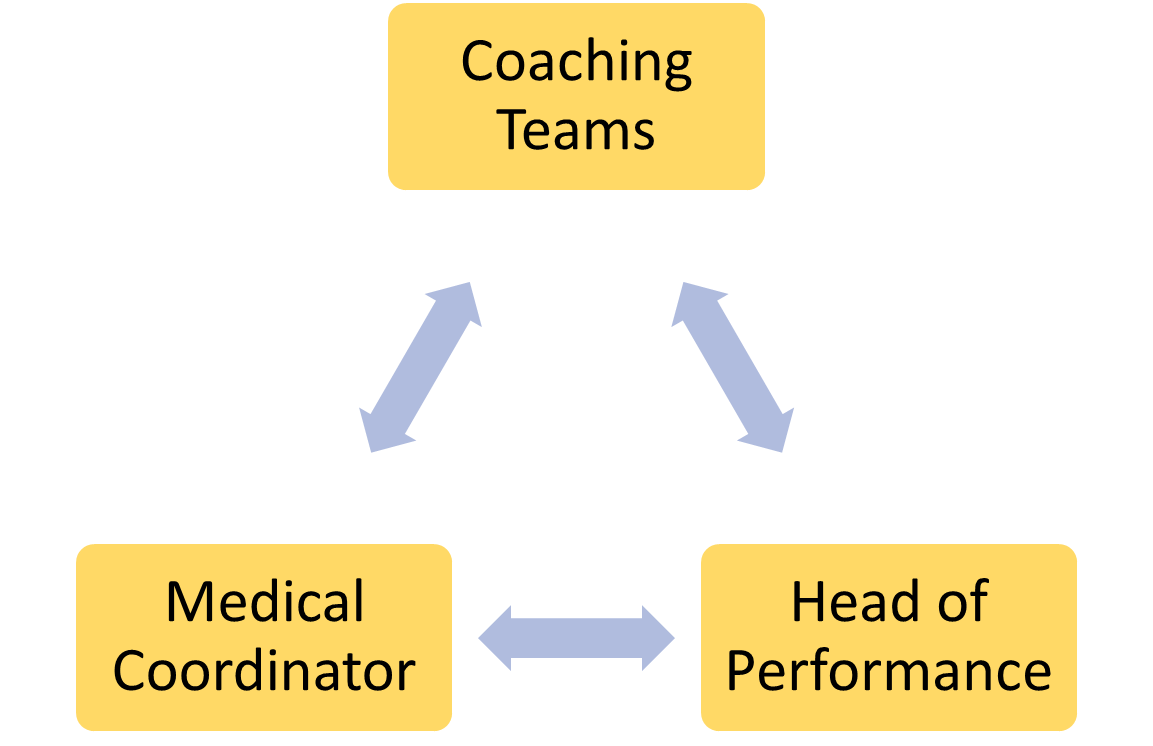
As strength and conditioning coaches, we combine sports science and coaching to reduce injuries and improve physical and athletic performance. Some rehab coaches focus on physical training, monitoring, and testing, while others use on field coaching skills to improve technical, tactical, and mental skills. I believe inter-discipline communication and integration are crucial for long-term athlete health care and decision-making to optimise the performance of that athlete from a physical to mental capacity. While our medical and coaching divisions operate independently, they collaborate in order to accomplish performance objectives. At our facility we are lucky to have a high-performance manager within the environment to establish clear and precise delineations of individual duties and obligations within every department. As a rehab coach, it is mandatory to possess a practical understanding of every discipline in order to discern when referrals are warranted and to recognise limitations within the scope of practice and knowing when to refer back for a medical review or surgical intervention. For instance, coaches ought to be well-informed regarding significant injuries and illnesses; physiotherapists should be conversant with the strength and conditioning requirements of the player; and physicians should be conversant with the physiological and mechanical demands of the sport.
Figure 2: The integration of Roles and responsibilities amongst an Interdisciplinary Team at Offaly GAA
.png)
Within the medical / performance team the aim is to decrease injury, sickness and optimise performance. This results in a combined and integrated injury prevention and performance system. The medical team provides evidence-based injury prevention solutions and early management of player / athlete symptoms alongside the rehabilitation and strength and conditioning coaches who understand the needs analysis of the athlete. The Gaelic Games injury scheme claims initiative has generated valuable evidence for injury surveillance allowing understanding of the most common GAA injuries ad potential mechanisms / strategies that could be implemented in reducing this risk.
Previous injury is the most significant factor in predicting hamstring injuries, with running being the most frequent cause of injury. We know throughout sport that there is high recurrence incidence of hamstring strain injuries which potentially indicates that existing preventative training programs and rehabilitation treatments are not sufficiently efficient. As Rehab Coaches, our primary responsibility is look at range of movement deficits, strength asymmetries, movement pattern dysfunction and build the athlete to optimise their performance prior to their return to play so that they were improved on where they were prior to their injury. However, early stage management of a hamstring strain should be overseen by a Physiotherapist with or without a referral pathway to a surgeon depending on the location of the hamstring injured and extent of the grade.
If there are specific gaps in the rehab coach’s ability then further referral to speed coaches or return to play specialists might be warranted to view the acceleration, deceleration, change of direction and max velocity running mechanics. I also refer to Nutritional and psychological clinicians to help with return to play as this additional strategy could help maximise the recovery process. The use of a collaborative strategy showcases how each profession is employing their distinct expertise to together pursue a shared objective. The need for multidisciplinary assistance for athletes has grown, leading to a rise in the likelihood of professional, ethical, and legal issues.
Working within an integrated health, performance and coaching approach necessitates the exchange of information concerning the athlete's
health. This gives rise to certain ethical quandaries about secrecy and the relationship between each party involved. In order
to address the matter of informed consent, our players are required to sign a statement that explicitly outlines our representation of the
team and the potential disclosure of any information pertaining to their medical or physical condition to relevant members of the medical,
performance and coaching team, if deemed suitable.
As a rehab coach I acknowledge the athlete as my client, but within the sport there is significant disparity in adherence to professional norms of behaviour. This can result in varying degrees of information being communicated to the coaching team. The Medical and Rehabilitation environment in elite settings is characterised by its logistical aspects and many challenges when it comes to maintaining confidentiality. Within a private clinic separate assessment or treatment rooms ensure patient anonymity. However, within the sports environment this sometimes is not feasible and poses issues with respect to confidentiality. As a Rehab coach I have direct contact with athletes, thus they have more chances to give information regarding their physical, mental and home life.
If the athlete presents an issue regarding their psychological health or for instance social drug issues etc then If the Rehab coach relaying this information to other medical personnel or the coaching team, it may affect the athlete's view of them and alter the relationship and trust. As a Rehab Coach, athletes may have confided in them but asked not to share the information with coaches or other staff. However, within the medical performance team it is required to share such information, but in doing so will damage the player's confidence. On a more drastic scale take the example of the Russian state sponsored doping program which is one of the most contentious events in modern sport. This shows how external pressure might cause clinicians to ignore professional norms and forfeit their professional ethics to retain their job.
Conclusion
Our governing bodies must stay abreast of policy and regulatory developments to deliver the best treatment in competitive sports. Our role goes beyond what is expected in other circumstances. Medical and Rehabilitation coaches confront ethical difficulties, but I think if you build rapport and create moral limits within the team, you should have a healthy working relationship. Professional honesty should guide all decisions.
Thanks for reading.... Chris



.jpg)