
Cardiac Arrest
At Physio Tullamore when identifying an athlete who has collapsed with a cardiac arrest, we immediately call for help, then check for safety and then start good quality cardiopulmonary resuscitation. The emphasis is particularly on good quality chest compressions at the correct rate and depth for the casualty.
Rescuer safety
It is essential that the members of the medical team ensure that it is safe to approach an ill or injured athlete. The SAFE approach is as follows:
• Shout for help
• Assess the scene
• Free from danger
• Evaluate the athlete
When entering the field of play, ensure your medical team know you are attending to a player and ensure that the officials are made aware. Is it safe, has play moved away or the game stopped? It is important to understand that safety is dynamic in time and place and not confined to a single assessment at the beginning of the incident.
When attending to injured players on the pitch, it is vital that correct clothing is worn for safety and ease of identification. Wearing a brightly coloured bib may assist in the officials being aware you are on the pitch. Wearing clinical gloves on both hands prior to the incident will save time in preparation when needing to attend to an athlete but also ensure protection of yourself, especially when dealing with bodily fluids, e.g. blood.
When considering CPR, in particular mouth-to-mouth, there are concerns that there is a risk of infection. To date, the risks of infection are:

• 15 documented cases of CPR related infection – mainly Neisseria meningitidis
• Tuberculosis
• No cases of hepatitis B or C, or CMV
• Three cases of HIV transmission from high-risk cutaneous exposure
Expired air ventilation using a pocket mask with oxygen attached. The best way to prevent the risk of any infection is to use a face shield or, ideally, a pocket mask. The added advantage of a pocket mask is that most of them have a nipple to which you can attach oxygen piping to increase the amount of oxygen being delivered to the casualty from the 16% contained in expired air.
Adult basic life support
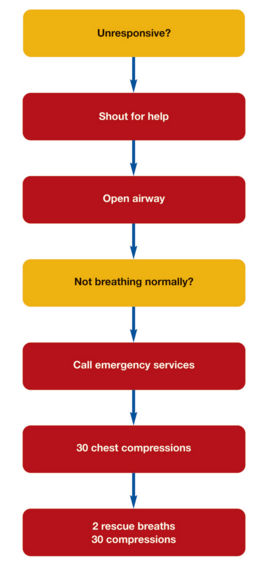
The algorithm shown above illustrates the important steps in assessing and delivering CPR to an arrested athlete. Of particular importance is the early call for help, ensuring help is on its way and a call for emergency services after recognising an athlete is not breathing.
Adult basic life support (continued)
In a non-traumatic collapse, the assessment of breathing is achieved by opening the airway with a head tilt chin lift manoeuvre and looking, listening and feeling for 10 seconds:
• Head tilt, chin lift
• If cervical spine injury suspected – jaw thrust
• Look for chest movement
• Listen for breath sounds
• Feel for expired air
• Assess for 10 seconds
When health care professionals are in attendance, a combined airway and pulse check can be performed. This allows for the identification of a respiratory only arrest with a pulse present. In this scenario, ventilations should be administered to the patient using a pocket mask or bag valve mask at a rate of 10-12 per minute, ensuring regular pulse checks are performed at least every minute.
When assessing the patient, if there are no breath sounds and no pulse, then chest compression should be commenced immediately, after ensuring emergency aid is on its way.
Adult basic life support (continued)
Chest compressions should be delivered in the centre of the chest, at a depth of 5-6 cm in adults and at a rate of 100-120 per minute. After 30 chest compressions, two ventilations should be delivered. These are delivered using the following steps:
• Blow steadily (1 second) into pocket mask or use a bag valve mask
• Allow chest to fall (1 second)
• Repeat breath/ventilation in (1 second)
• Allow chest to fall (1 second)
• Total for two breaths is 4 -5 seconds
• Minimal interruption to CPR
• Watch for the chest to rise
• Maintain the chin lift/jaw thrust
• Watch the chest fall


The key to this is ensuring the patient’s airway is open to deliver the breaths/ventilations and ensure no longer than 4-5 seconds are spent delivering the ventilation, thus reducing the interruption to chest compressions and maintaining cardiac artery perfusion pressure. Thereafter, 30 compressions should be delivered before each two breaths/ventilations are delivered.
If there is a reluctance to perform mouth-to-mouth/mouth to mask/bag valve mask ventilation, then chest compression alone is better than no CPR. CPR should be continued until help arrives and takes over, the victim starts breathing adequately for themselves or the rescuers become exhausted.
Paediatric basic life support
It is often asked at what age a responder should use the paediatric rather than adult algorithm. This is usually used if the patient is pre-pubertal.
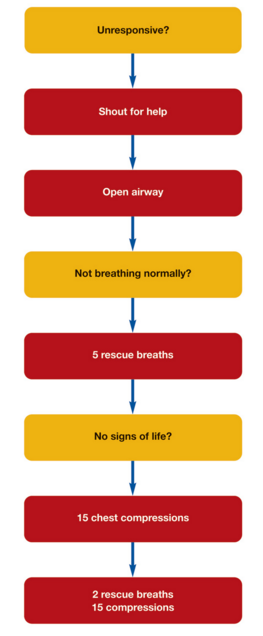
The paediatric life support algorithm shown above is similar to that of the adult algorithm. The main differences are that, on identifying the paediatric patient is not breathing, 5 rescue breaths/ventilations should be delivered before checking for further signs of life, e.g. a pulse. If after the 5 rescue breaths/ventilations have been delivered and there is no sign of life, then then 15 chest compressions should be administered.
In a child, these are delivered at a depth of 5cm, while in an infant, it is 4cm. The rate of compressions remains at 100-120 per minute but the ratio of compressions to breathes is 15 compressions to 2 breathes.
At Physio Tullamore we are qualified in trauma management. If you have any queries about this blog please feel free to drop me a message.
Thanks
Physio Tullamore


.jpg)