Secondary Headaches:
Headaches belonging to this category have an underlying condition that at times can be ominous and life-threatening. They have similar
criteria to that of Primary headaches but have causation by another disorder and include the following:
1. Headache attributed to trauma or injury to the head and/or neck
2. Headache attributed to cranial or cervical vascular disorder
3. Headache attributed to non-vascular intracranial disorder
4. Headache attributed to a substance or its withdrawal
5. Headache attributed to infection
6. Headache attributed to disorder of homoeostasis
7. Headache or facial pain attributed to disorder of the cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cervical
structure
8. Headache attributed to psychiatric disorder
Secondary headaches are attributed to a causative disorder such as a vascular, inflammatory, traumatic or neoplastic aetiology. However,
medication overuse headache as shown to outnumber other causes, and may can result in large morbidity if left untreated.
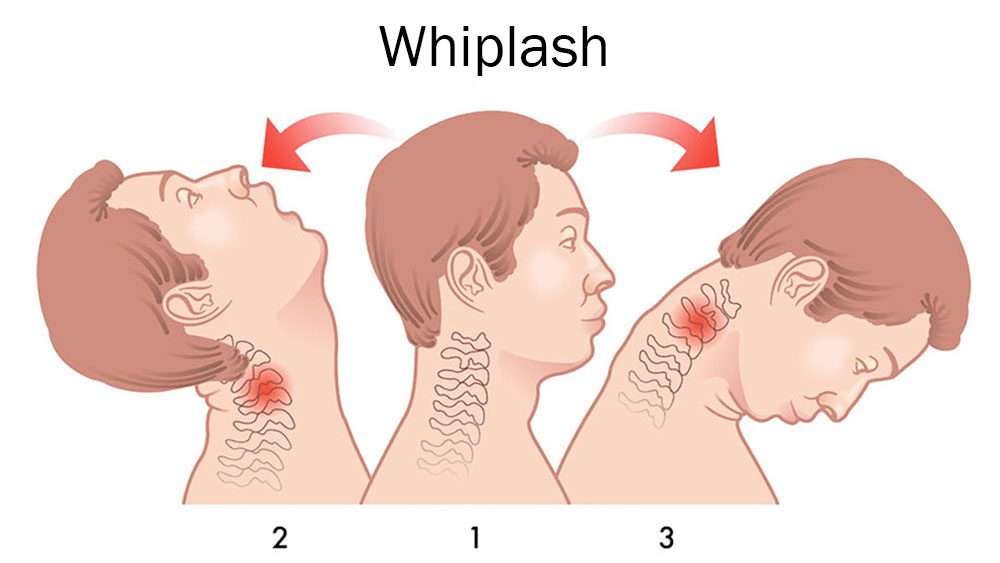
Post traumatic headaches related to trauma of head and or neck, whiplash or related cranial trauma are classified as acute if occurring
within one week following inciting event or following returning consciousness or ceasing medications which would impair judgement or
reporting of headache.
Headache associated with stroke (ischemic and haemorrhagic), arterial bleeding, arteritis, cerebral venous sinus thrombosis (CVST), genetic
vasculopathies or post-procedural headaches tend to present acutely with neurological signs and symptoms. All these conditions may occur in
patients who have previously been affected by types of primary headaches. The onset of a new headache which reports to be of very strong
intensity (worst ever) is a key underlying factor of a vascular condition and should be diagnosed using the following criteria:
1. Headache fulfilling criterion the list above
2. A cranial and/or cervical vascular disorder known to be able to cause headache has been demonstrated
3. Evidence of causation demonstrated by at least two of the following:
headache has developed in temporal relation to the onset of the cranial and/or cervical vascular disorder
▪either or both of the following: –
headache has significantly worsened in parallel with worsening of the cranial and/or cervical vascular disorder –
headache has significantly improved in parallel with improvement of the cranial and/or cervical vascular disorder
▪headache has characteristics typical for the cranial and/or cervical vascular disorder
▪other evidence exists of causation