
Athletic Groin Pain in Sport
Overview:
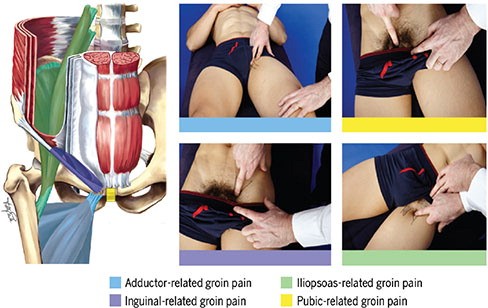
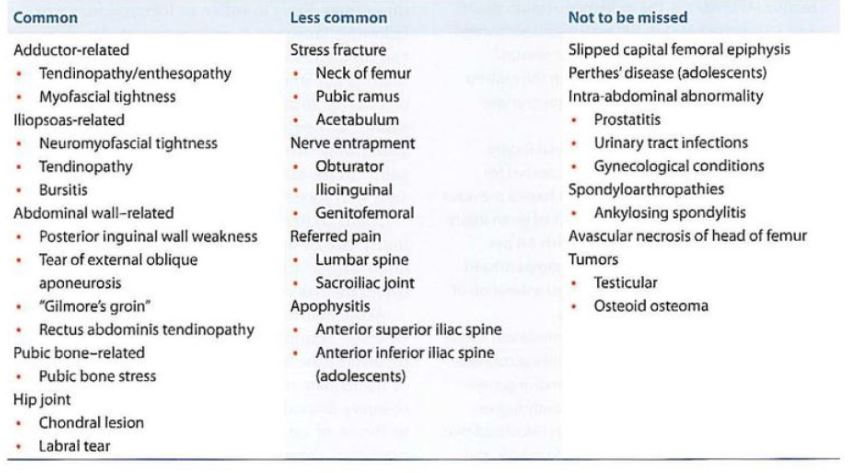
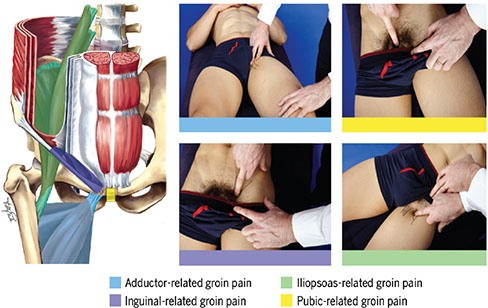
Groin pain in athletes that is not associated with the hip joint is often referred to by various terms, such as athletic pubalgia, sports hernia, and adductor tendinopathy. The 2015 Doha Agreement categorized this pain into three main groups: (1) defined clinical entities (adductor-related, inguinal-related, iliopsoas-related, and pubic-related), (2) hip-related groin pain, and (3) other causes like true inguinal hernias and non-musculoskeletal conditions (Weir et al., 2015). Terms like "athletic pubalgia" and "sports hernia" are being phased out in favour of more specific classifications. Groin Pain in Athletes (Non-Hip Joint)

Classification of Groin Pain:
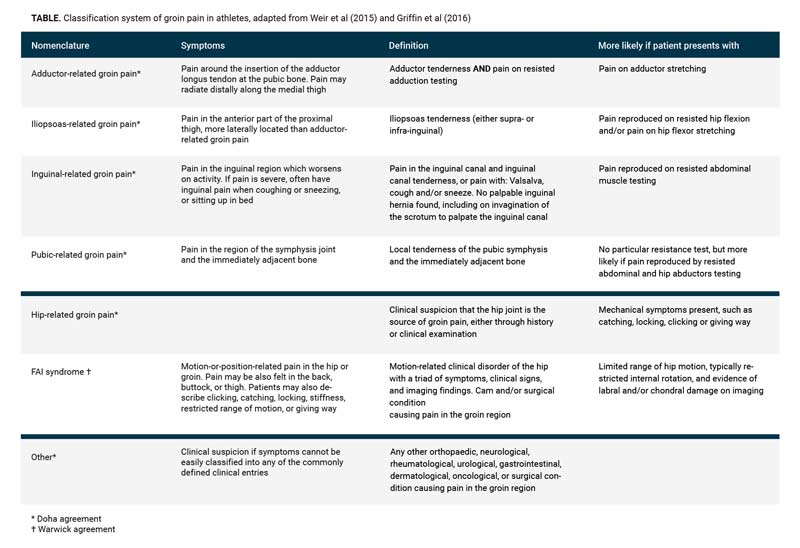
The Anatomy of the Athletic Groin
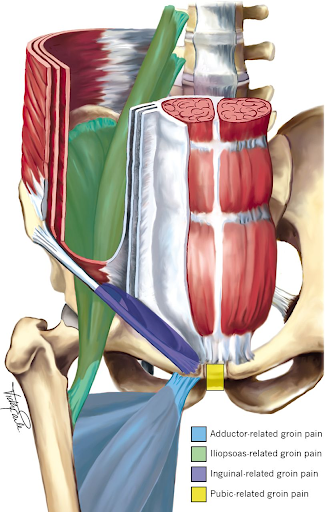
The interactions among the abdominal wall, hip joint, sacroiliac joint, adductors, and pubic symphysis are
intricate. A notable imbalance in forces between the abdominal muscles and adductors can lead to microtrauma in the fascia. Proper
classification aids in pinpointing and conveying the location of this microtrauma. For instance, inguinal-related groin pain manifests as
pain and tenderness concentrated around the inguinal canal, stemming from microtrauma to the posterior inguinal canal, which may or may not
involve nerve compression. Similarly, iliopsoas-related groin pain arises from microtrauma to the iliopsoas muscle.
Hip pathologies often result in a limited range of motion (ROM). To attain adequate ROM for athletic activities, compensatory stretching of
the surrounding muscles occurs, which makes these tissues more susceptible to microtrauma and force imbalances. The treatment approaches for
intra-articular hip pathologies differ from those addressing extra-articular issues, thus necessitating a separate categorization for
hip-related groin pain.
Regarding non-hip groin pain, literature indicates a significant diversity in pathology within a relatively small anatomical region. A
2020 review published in JAMA Surgery outlined several pathological origins of groin pain syndromes, including the inguinal canal,
rectus abdominus, adductor longus, pubic symphysis, and inguinal neuralgia. These neuralgia may arise as a result of true hernias,
disruption of the transversalis fascia that increases pressure on the nerves, or entrapment due to scar tissue.
Common diagnosis of the Groin
The Pubic Clock
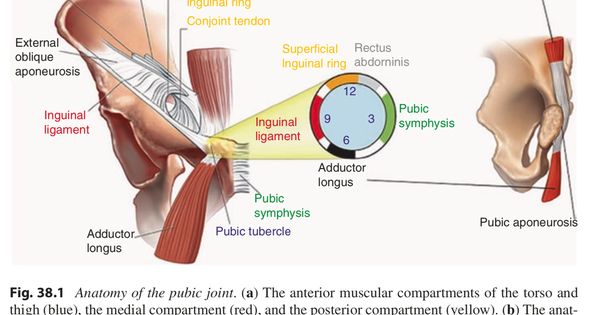
An important anatomical feature of the pubis is its role as a central point for the attachments of various structures, including the rectus abdominis, adductor longus, inguinal ligament, and conjoint tendon . This region of the pubis is located just lateral to the pubic symphysis. A study by Falvey et al. (2016) involving 382 male athletes suffering from groin pain, primarily Gaelic football players, found that 68% had bone marrow edema, and 52.6% showed abnormalities in the pubic aponeurosis on MRI. Nearly one-third of the patients exhibited three or more findings on their MRI scans. Additionally, research by Schilders et al. (2017) identified a pubic ligament complex within the pubic aponeurosis. This ligament runs horizontally at the midline and connects with the pyramidalis and adductor tendons as well as the external oblique aponeurosis, lying just above the rectus abdominis. The goal of assessing groin pain is to systematically rule out different diagnoses and narrow down the differential through thorough examination. The wide variation in non-hip joint-related groin pain suggests that it likely has multiple contributing factors.
Examination:
At Offaly Physio & Performance Lab we use comprehensive examination for groin pain (inguinal-related, pubic-related, adductor-related and psoas-related) must involve examination to exclude intra-articular hip pain, inguinal, femoral, and spigelian hernias, as well as the pubic bone (superior and inferior ramus), pubic symphysis, and other soft-tissues injuries. Strength testing using force frames can be beneficial to ascertaining strength assymetries between sides.

When to Use Imaging?
Investigations:
-
X-ray:
Views include AP Pelvis, lateral hip, and Dunn views.
-
Abdominal Ultrasound (US):
Primarily used to rule out other hernias.
-
Dynamic US for Sports Hernia:
A positive finding is the bulging of the posterior inguinal wall (transversus abdominis) when the patient performs the Valsalva maneuver.
-
CT Scan:
Assesses the hips and pubic symphysis with some capacity to evaluate soft tissue scarring.
-
MRI Groin Pain Protocol:
Evaluates the hip, psoas, proximal rectus femoris, inguinal ligament, pubic rami, and symphysis.
-
MR Neurography:
Used to detect impingement of the iliohypogastric, ilioinguinal, and genitofemoral nerves.
Plan:
Prognosis:
Determining prognosis is challenging due to the variety of conditions. Return-to-play timelines vary significantly, ranging from 2 to 30
weeks, according to a 2015 review by King et al. For pubic-related pain, recovery with rehabilitation is notably faster than with surgery,
with an approximate 12-week difference. For abdominal and adductor-related pain, no significant differences were observed between surgical
and non-surgical treatments. Across all studies, the average return to play was 13 weeks. Age influences prognosis, with younger patients in
their 20s recovering faster than those over 40. In a 2011 study by Paajanen et al., 53% of the non-operative group continued to have
symptoms after one year, despite physiotherapy and anti-inflammatory treatments. The presence of bone marrow edema ("osteitis pubis") on MRI
often leads to longer recovery periods, typically over three months.
Conservative Management:
Rehabilitation varies by the underlying pathology but often involves improving hip range of motion and lumbopelvic control.
-
Abdominal-related pain:
A 4-week protection phase from excessive tension is recommended, followed by 4-6 weeks of gradual muscle activation, focusing on hip range of motion and core mobility. Return to agility training should be avoided until at least 4 weeks without pain.
-
Adductor-related pain:
Avoid aggravating activities with a gradual strengthening program, emphasizing hip mobility and core strength.
-
Inguinal-related pain:
A 4-week protection phase similar to abdominal pain, with a gradual return to muscle activation and hip/core training.
-
Pubic-related pain:
The same 4-week protection phase applies, with a focus on controlled muscle activation. A minimum of four pain-free weeks is advised before resuming agility drills.
Injections:
Adjunct treatments include NSAIDs and injections (corticosteroids or platelet-rich plasma) into the pubic symphysis or rectus abdominis
muscles.
Radiofrequency Ablation/Denervation:
In cases of nerve-like symptoms or pain spanning the inguinal, pubic, or adductor areas, nerve blocks may be useful both diagnostically and
therapeutically. Radiofrequency ablation (RFA) of the ilioinguinal nerve has shown promise, with improvement in studies comparing it to
local anesthetics. A notable case involved a professional football player achieving full recovery after iliohypogastric nerve RFA.
Surgical Management:
There are various surgical approaches, including the fixation of the transversus abdominis to the inguinal ligament, mesh insertion,
adductor tenotomy, rectus abdominis repair, and nerve neurectomy.
-
Adductor tenotomy: Generally reserved for chronic, localized adductor pain. Robertson et al. (2011) reported a 71% return
to pre-injury levels in athletes after chronic adductor pain surgery.
-
Laparoscopic mesh repair: Frequently used for posterior wall defects, with studies showing high success rates (97% return
to sport within three weeks) in athletes.
-
Open repair: A technique involving posterior wall repair with decompression of the genital branch of the genitofemoral
nerve. In one study, 84% of patients returned to their pre-injury activity level within four weeks.
Complications:
Common complications include bruising, bleeding, hematomas, infections, and nerve-related issues (dysthesias).
Criteria for Referral for Laparoscopic Repair for Sports Hernia:
History (All three must be present):
- Athletic injury with overuse or gradual onset.
- Symptoms worsened by twisting, sprinting, or directional changes.
- Pain persisting for over 6 months (or 6 weeks in elite athletes).
Examination (Both must be present):
- Pain over the inguinal ligaments and at the internal/external rings.
- No evidence of a true inguinal hernia.
Imaging (Both must be present):
- Ultrasound shows no true inguinal hernia.
- MRI Groin Pain Protocol negative for other causes.
Note:
Despite favorable surgical outcomes, access to such interventions may be geographically limited.
Thank you for reading this blog
If you would like to book an appointment to review your groin pain please feel free to do so
www.offalyphysioandperformancelab.com/book-online
References
- Drager J, Rasio J, Newhouse A. Athletic Pubalgia (Sports Hernia): Presentation and Treatment. Arthroscopy. 2020 Dec;36(12):2952-2953.
- Emblom BA, Mathis T, Aune K. Athletic Pubalgia Secondary to Rectus Abdominis-Adductor Longus Aponeurotic Plate Injury: Diagnosis, Management, and Operative Treatment of 100 Competitive Athletes. Orthop J Sports Med. 2018 Sep 24;6(9):2325967118798333.
- King E, Franklyn-Miller A, Richter C, O’Reilly E, Doolan M, Moran K, Strike S, Falvey É. Clinical and biomechanical outcomes of rehabilitation targeting intersegmental control in athletic groin pain: prospective cohort of 205 patients. Br J Sports Med. 2018 Aug;52(16):1054-1062.
- Falvey ÉC, King E, Kinsella S, Franklyn-Miller A. Athletic groin pain (part 1): a prospective anatomical diagnosis of 382 patients–clinical findings, MRI findings and patient-reported outcome measures at baseline. Br J Sports Med. 2016 Apr;50(7):423-30.
- Franklyn-Miller A, Richter C, King E, Gore S, Moran K, Strike S, Falvey EC. Athletic groin pain (part 2): a prospective cohort study on the biomechanical evaluation of change of direction identifies three clusters of movement patterns. Br J Sports Med. 2017 Mar;51(5):460-468.
- Choi H, McCartney M, Best TM. Treatment of osteitis pubis and osteomyelitis of the pubic symphysis in athletes: a systematic review. Br J Sports Med. 2011 Jan;45(1):57-64.
- McKim KR, Taunton JE. The effectiveness of compression shorts in the treatment of osteitis pubis. NZ J Sports Med 2001: 29: 70–73.
- Topol GA, Reeves KD, Hassanein KM. Efficacy of dextrose prolotherapy in elite male kicking‐sport athletes with chronic groin pain. Arch Phys Med Rehabil 2005: 86: 697–702.
- St-Onge E, MacIntyre IG, Galea AM. Multidisciplinary approach to non-surgical management of inguinal disruption in a professional hockey player treated with platelet-rich plasma, manual therapy and exercise: a case report. J Can Chiropr Assoc. 2015;59(4):390-397.
- Scholten PM, Massimi S, Dahmen N, Diamond J, Wyss J. Successful treatment of athletic pubalgia in a lacrosse player with ultrasound-guided needle tenotomy and platelet-rich plasma injection: a case report. PM R. 2015 Jan;7(1):79-83.
- Topol GA, Reeves KD. Regenerative injection of elite athletes with career-altering chronic groin pain who fail conservativetreatment: a consecutive case series. Am J Phys Med Rehabil 2008 Nov; 87 (11): 890–902
- King E, Ward J, Small L, et al. Athletic groin pain: a systematic review and meta-analysis of surgical versus physical therapy rehabilitation outcomes. British Journal of Sports Medicine 2015;49:1447-1451.
- Hiti, C.J., Stevens, K.J., Jamati, M.K. et al. Athletic Osteitis Pubis. Sports Med 2011;41:361–376.
- Gerhardt M, Christiansen J, Sherman B, Miranda A, Hutchinson W, Chahla J. Outcomes following surgical management of inguinal-related groin pain in athletes: a case series. J Hip Preserv Surg. 2020 Jan 22;7(1):103-108.
- “Athletic Pubalgia/Core Muscle Injury and Adductor Pathology.” DeLee & Drez’s Orthopaedic Sports Medicine, by Mark D. Miller and Stephen R. Thompson, Elsevier, 2019, pp. 1007–1017
- http://sportmedschool.com/journal-club/sports-hernia-wheres-the-hernia/
- Clelland AD, Varsou O. A qualitative literature review exploring the role of the inguinal ligament in the context of inguinal disruption management. Surg Radiol Anat. 2019 Mar;41(3):265-274. doi: 10.1007/s00276-018-2170-6. Epub 2018 Dec 20. PMID: 30570676; PMCID: PMC6420487.
- Poh F, Xi Y, Rozen SM, Scott KM, Hlis R, Chhabra A. Role of MR Neurography in Groin and Genital Pain: Ilioinguinal, Iliohypogastric, and Genitofemoral Neuralgia. AJR Am J Roentgenol. 2019 Mar;212(3):632-643. doi: 10.2214/AJR.18.20316. Epub 2019 Jan 8. PMID: 30620677.
- Cirocchi R, Mercurio I, Nazzaro C, De Sol A, Boselli C, Rettagliata G, Vanacore N, Santoro A, Mascagni D, Renzi C, Lancia M, Suadoni F, Zanghì G, Palumbo P, Bruzzone P, Tellan G, Fedeli P, Marsilio F, D’Andrea V. Dermatome Mapping Test in the analysis of anatomo-clinical correlations after inguinal hernia repair. BMC Surg. 2020 Dec 7;20(1):319. doi: 10.1186/s12893-020-00988-1. PMID: 33287793; PMCID: PMC7720581.
- http://www.groinpainclinic.co.uk/groin-pain/nerves-affected-in-chronic-groin-pain – Figure 4
- Elattar O, Choi HR, Dills VD, Busconi B. Groin Injuries (Athletic Pubalgia) and Return to Play. Sports Health. 2016 Jul;8(4):313-23. doi: 10.1177/1941738116653711. Epub 2016 Jun 14. PMID: 27302153; PMCID: PMC4922526.
- Muschaweck UU, Berger LML (2010) Sportsmen’s groin-diagnostic approach and treatment with the minimal repair technique: a single-center uncontrolled clinical review. Sports Health 2(3):216–221
- Sheen AJ, Stephenson BM, Lloyd DM, Robinson P, Fevre D, Paajanen H, de Beaux A, Kingsnorth A, Gilmore OJ, Bennett D, Maclennan I, O’Dwyer P, Sanders D, Kurzer M. Treatment of the sportsman’s groin’: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference. Br J Sports Med. 2014 Jul;48(14):1079-87. doi: 10.1136/bjsports-2013-092872. Epub 2013 Oct 22.
- Ellsworth AA, Zoland MP, Tyler TF. Athletic pubalgia and associated rehabilitation. Int J Sports Phys Ther. 2014 Nov;9(6):774-84.
- Šebečić B, Japjec M, Janković S, Vencel Čuljak, Dojčinović B, Starešinić M. Is chronic groin pain a Bermuda triangle of sports medicine? Acta Clin Croat. 2014 Dec;53(4):471-8.
- Omar IM, Zoga AC, Kavanagh EC, Koulouris G, Bergin D, Gopez AG, Morrison WB, Meyers WC. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. 2008 Sep-Oct;28(5):1415-38. doi: 10.1148/rg.285075217. Review.
- Kopelman D, Kaplan U, Hatoum OA, Abaya N, Karni D, Berber A, Sharon P, Peskin B The management of sportsman’s groin hernia in professional and amateur soccer players: a revised concept. Hernia. 2014 Nov 8
- Rambani R, Hackney R. Loss of range of motion of the hip joint: a hypothesis for etiology of sports hernia. Muscles Ligaments Tendons J. 2015 Mar 27;5(1):29-32. eCollection 2015 Jan-Mar.
- Srinivasan A, Schuricht A (2002) Long-term follow-up of laparoscopic preperitoneal hernia repair in professional athletes.J Laparoendosc Adv Surg Tech 12(2):101–106
- Steele P, Annear P, Grove JR (2004) Surgery for posterior inguinal wall deficiency in athletes. J Sci Med Sport 7(4): 415–421 discussion 422–3\
- Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR (2000) Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med 28(1):2–8
- Meyers WC, Lanfranco A, Castellanos A (2002) Surgical management of chronic lower abdominal and groin pain in high performance athletes. Curr Sports Med Rep 1(5):301–305
- Paajanen H, Brinck T, Hermunen H, Airo I (2011) Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: a randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia). Surgery 150(1):99–107
- Paajanen H, Heikkinen J, Hermunen H, Airo I. Successful treatment of osteitis pubis by using totally extraperitoneal endoscopic technique. Int J Sports Med. 2005;26:303-306.
- Genitsaris M, Goulimaris I, Sikas N (2004) Laparoscopic repair of groin pain in athletes. Am J Sports Med 32(5):1238–1242
- Santilli OL, Nardelli N, Santilli HA, Tripoloni DE.Sports hernias: experience in a sports medicine center. Hernia. 2015 Mar 18.
- Verrall GM, Slavotinek JP, Fon GTIncidence of pubic bone marrow oedema in Australian rules football players: relation to groin painBritish Journal of Sports Medicine 2001;35:28-33.
- Verrall GM, Hamilton IA, Slavotinek JP, Oakeshott RD, Spriggins AJ, Barnes PG, Fon GT. Hip joint range of motion reduction in sports-related chronic groin injury diagnosed as pubic bone stress injury. J Sci Med Sport. 2005 Mar;8(1):77-84. doi: 10.1016/s1440-2440(05)80027-1. PMID: 15887904.
- Serner A, van Eijck CH, Beumer BR, et alStudy quality on groin injury management remains low: a systematic review on treatment of groin pain in athletesBritish Journal of Sports Medicine 2015;49:813.
- Serner A, Weir A, Tol JL, Thorborg K, Roemer F, Guermazi A, Yamashiro E, Hölmich P. Characteristics of acute groin injuries in the adductor muscles: A detailed MRI study in athletes. Scand J Med Sci Sports. 2018 Feb;28(2):667-676. doi: 10.1111/sms.12936. Epub 2017 Jul 26. PMID: 28649700.
- Schilders E, Bharam S, Golan E, Dimitrakopoulou A, Mitchell A, Spaepen M, Beggs C, Cooke C, Holmich P. The pyramidalis-anterior pubic ligament-adductor longus complex (PLAC) and its role with adductor injuries: a new anatomical concept. Knee Surg Sports Traumatol Arthrosc. 2017 Dec;25(12):3969-3977. doi: 10.1007/s00167-017-4688-2. Epub 2017 Sep 2. PMID: 28866812; PMCID: PMC5698379.
- Brown, Rea A MD; Mascia, Anthony MD; Kinnear, Douglas G MD; Lacroix, Vincent MD; Feldman, Liane MD; Mulder, David S MD An 18-Year Review of Sports Groin Injuries in the Elite Hockey Player: Clinical Presentation, New Diagnostic Imaging, Treatment, and Results, Clinical Journal of Sport Medicine: May 2008 – Volume 18 – Issue 3 – p 221-226 doi: 10.1097/JSM.0b013e318172831a
- Jardí J, Rodas G, Pedret C, Til L, Cusí M, Malliaropoulos N, Del Buono A, Maffulli N. Osteitis pubis: can early return to elite competition be contemplated? Transl Med UniSa. 2014 Apr 8;10:52-8. PMID: 25147768; PMCID: PMC4140431.
- Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. . Experience With “Sports Hernia” Spanning Two Decades. Annals of Surgery. 2008;248(4):656-665. doi: 10.1097/SLA.0b013e318187a770.
- Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, Khan KM, et al. . Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med. (2015) 49:768–74. 10.1136/bjsports-2015-094869.
- Susmallian S, Ezri T, Elis M, Warters R, Charuzi I, Muggia-Sullam M. Laparoscopic repair of ‘sportsman’s hernia’ in soccer players as treatment of chronic inguinal pain. Med Sci Monit. 2004;10:52-54.
- Comin J, Obaid H, Lammers G, Moore J, Wotherspoon M, Connell D. Radiofrequency denervation of the inguinal ligament for the treatment of ‘Sportsman’s Hernia’: a pilot study. Br J Sports Med. 2013 Apr;47(6):380-6. doi: 10.1136/bjsports-2012-091129. Epub 2012 Sep 5. PMID: 22952407.
- Zuckerbraun BS, Cyr AR, Mauro CS. Groin Pain Syndrome Known as Sports Hernia: A Review. JAMA Surg. 2020;155(4):340–348. doi:10.1001/jamasurg.2019.5863
- Robertson IJ, Curran C, McCaffrey N, Shields CJ, McEntee GP. Adductor tenotomy in the management of groin pain in athletes. Int J Sports Med. 2011 Jan;32(1):45-8. doi: 10.1055/s-0030-1263137. Epub 2010 Nov 25. PMID: 21110286.


.jpg)